 Launched in February 2019, the Morris Hospital Integrated Behavioral Health program has been working to address a growing need for behavioral health resources within the primary care setting.
Launched in February 2019, the Morris Hospital Integrated Behavioral Health program has been working to address a growing need for behavioral health resources within the primary care setting.
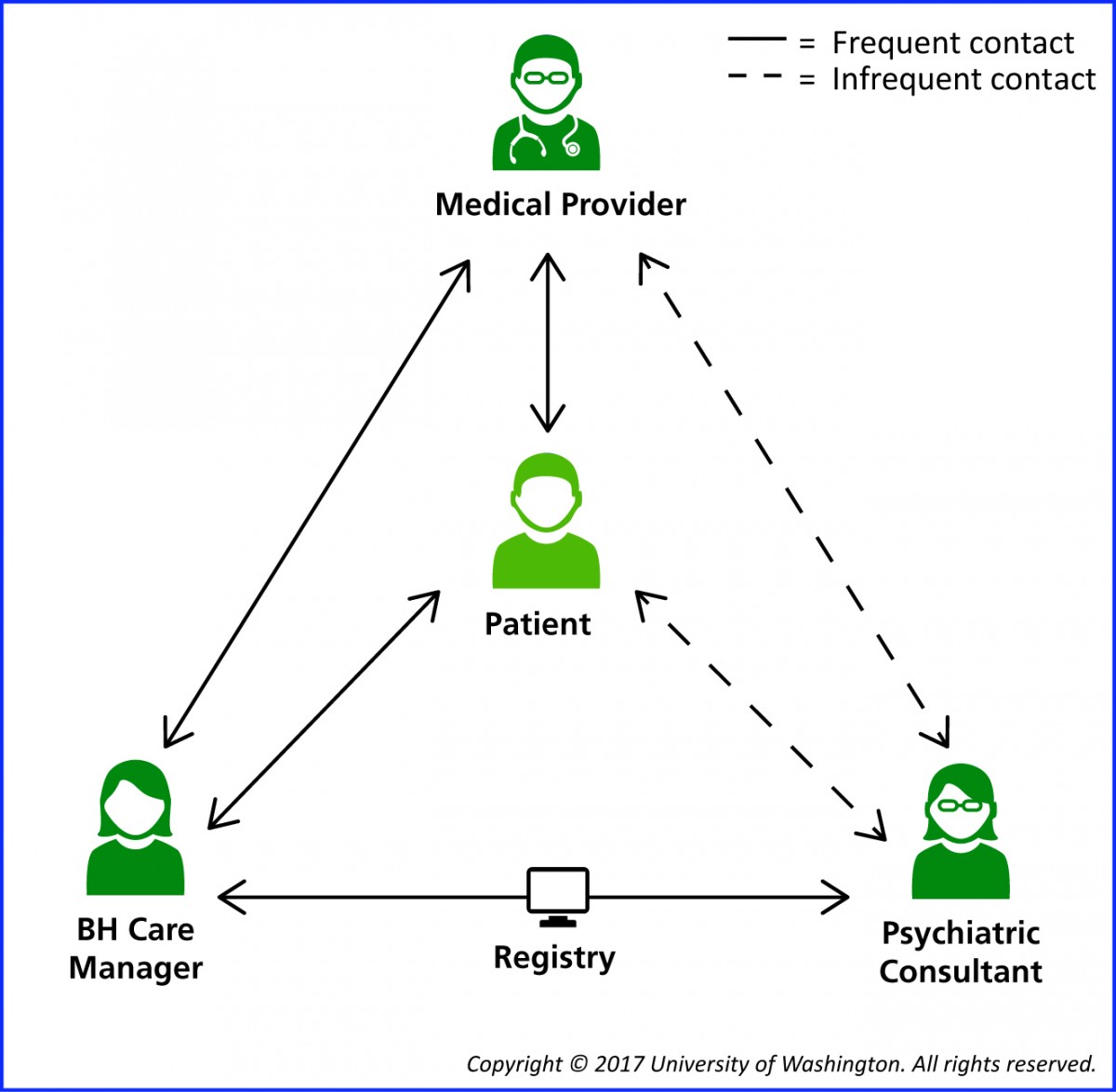
Morris Hospital has adopted the Collaborative Care Model (CoCM), which is team-based behavioral health delivered in the primary care setting. CoCM involves three team members: a primary care provider, a behavioral care coordinator and a consulting psychiatrist. This team-based care program embraces a philosophy of addressing whole-person needs rather than treating medical and mental health needs separately.
This means patients can receive care through their primary care provider for behavioral and mental health conditions such as:
- Depression
- Anxiety
- Bipolar Disorder
- Post-Traumatic Stress Disorder
- Addictions
- Substance Use Disorder
WHAT IS INTEGRATED BEHAVIORAL HEALTH?
Integrated behavioral health is the connection between a person’s health and well-being of the body and the mind. Behavioral health issues can include mental or psychiatric conditions, marriage and family issues, and substance use disorders.
According to the American Hospital Association, behavioral health disorders affect nearly one in five Americans and have community-wide impacts. Despite the prevalence of these disorders, a study showed that only 43 percent of the 44.7 million adults with mental health disorders received treatment, and less than 11 percent of adults with a substance use disorder received treatment.
HOW DO I GET TREATMENT?
If you are experiencing any behavioral health concerns, bring these concerns to your primary care provider. Morris Hospital is actively working to expand access to Collaborative Care at more of our locations. Currently, the primary care providers at the locations below work with a Collaborative Care team. Patients can begin the process by making an appointment with the primary care provider.
PRIMARY CARE LOCATIONS
The Primary Care Provider (PCP) oversees all aspects of your care at the clinic. He or she will work closely with the other members of the care team to make sure you get the best care possible. The PCP will make and/or confirm your diagnosis and may write or recall prescriptions for medications. The PCP works closely with your care manager to stay informed about your treatment progress. The PCP may also consult with the team psychiatrist if there are questions about the best treatments for you.
CHANNAHON
Channahon Healthcare Center of Morris Hospital
25259 Reed Street
Channahon, IL 60410
Phone: 815.467.0555
Providers: Dr. Mary Connolly, Sarah Bojak, F.N.P.
Morris Hospital Ridge Road Campus
27240 W. Saxony Dr., Suite 202
Channahon, IL 60410
Phone: 815.467.1518
Providers: Dr. Faiz Rahman, Dr. Lawton Moy, Dr. Scott Ciechna, Sherri Davis, P.A., Sarah Pettry-Soto, F.N.P.
GARDNER
Gardner Healthcare Center of Morris Hospital
409 N. Route 53
Gardner, IL 60424
Phone: 815.237.0413
Providers: Dr. Jennifer Thomas, Kathy Ulivi, F.N.P.
MINOOKA
Minooka Healthcare Center of Morris Hospital
603 W. Mondamin St.
Minooka, IL 60447
Phone: 815.521.1010
Providers: Dr. Hassnain Syed, Angela Todd, F.N.P.
MARSEILLES
Marseilles Healthcare Center of Morris Hospital
580 Sycamore Street
Marseilles, IL 61341
Phone: 815.795.2122
Providers: Dr. Ian Best, M.D.; Ashley Blough, F.N.P.-B.C.
MORRIS
Morris Healthcare Center of Morris Hospital
1300 W. Dresden Drive
Morris, IL 60450
Phone: 815.942.5200
Providers: Dr. Brad Lawton, Dr. Peter Roumeliotis, Dr. Olga Peplos, Diana Olsen, F.N.P., Diane Zuelke, F.N.P.
Morris Healthcare Center of Morris Hospital
151 W. High Street (Upper Level)
Morris, IL 60450
Phone: 815.705.3300
Providers: Dr. Ian Best, M.D.; Dr. Melissa Hill, M.D.; Dr. Faiz Rahman, M.D.
Morris Hospital Obstetrics & Gynecology Specialists
237 W. Waverly St.
Morris, IL 60450
Phone: 815.941.0441
Providers: Dr. Andrea Chen, Dr. Mary Fitzgibbon, Dr. Victoria Ochoa, Dr. Douglas Toussaint, Dr. Leticia Setrini-Best, Heidi Miller, N.P.
OTTAWA
Morris Hospital Ottawa Campus
1306 Gemini Circle, Suite 1
Ottawa, IL 61350
Phone: 815.433.9200
Providers: Dr. Hassnain Syed, Dr. Jeffrey Tanzi, Ashley Blough, F.N.P., Angela Todd, F.N.P.
SENECA
Seneca Healthcare Center of Morris Hospital
271 N. Main Street
Seneca, IL 61360
Phone: 815.357.8511
Providers: Dr. Colin Kao; Nina Seplak, F.N.P.
BEHAVIORAL CARE COORDINATORS
The Behavioral Care Coordinator works closely with you and the primary care provider (PCP) to implement a treatment plan. The Behavioral Care Coordinator answers questions about your treatment. He or she will check in with you to keep track of your treatment progress and can help identify side effects if you are taking medications. The PCP and the Behavioral Care Coordinator work together with you if a change in your treatment is needed. The Behavioral Care Coordinator may also provide counseling techniques proven to work in the primary care setting, such as Behavioral Activation and Problem Solving Therapy.
DAWN HARRIS, LCSW
 Dawn Harris is a Licensed Clinical Social Worker who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center – Mondamin Street and Morris Hospital Ottawa Campus.
Dawn Harris is a Licensed Clinical Social Worker who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center – Mondamin Street and Morris Hospital Ottawa Campus.
Dawn has been employed at Morris Hospital as a Behavioral Care Coordinator since July 2020. She earned her master’s degree from Loyola University Chicago and her bachelor’s degree from Northeastern Illinois University in Chicago. She has been counseling adults for more than 16 years.
Dawn believes in the collaborative care model as it provides patients an opportunity to receive care for mental health symptoms in a primary care setting, therefore, breaking down barriers to treatment and providing patients an opportunity to improve their lives by treating all aspects of their health.
SHERYL JANZ, LCPC
 Sheryl Janz is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center at the Morris Hospital Ridge Road Campus.
Sheryl Janz is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center at the Morris Hospital Ridge Road Campus.
Sheryl has been employed at Morris Hospital as a Behavioral Care Coordinator since May 2019. She has a master’s degree and bachelor’s degree from Lewis University in Romeoville and has been counseling adults and adolescents for more than 20 years.
Sheryl is passionate about Collaborative Care Counseling and finds the comprehensive, short-term model to be very effective in providing integrated care and improving clinical outcomes for patients.
KATRINA NEUBAUER, LCPC
 Katrina Neubauer is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for Morris Hospital Obstetrics & Gynecology Specialists.
Katrina Neubauer is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for Morris Hospital Obstetrics & Gynecology Specialists.
Katrina started with Morris Hospital in 2023. She completed her bachelor’s degree in psychology at Saint Xavier University and her master’s degree in clinical counseling psychology from Lewis University in Romeoville. Katrina has over 10 years of experience working with adults, adolescents, and children treating numerous mental health struggles in a variety of settings.
Katrina is passionate about the Collaborative Care Model as it unites physical and mental health concerns and integrates providers to deliver consistent care, along with improving the overall health of patients.
ASHLEY NORKUS, LCPC
 Ashley Norkus is a Licensed Clinical Professional Counselor who serves as the behavioral health care coordinator for the Morris Healthcare Center-Dresden Drive.
Ashley Norkus is a Licensed Clinical Professional Counselor who serves as the behavioral health care coordinator for the Morris Healthcare Center-Dresden Drive.
Ashley started with Morris Hospital in 2023. She completed her bachelor’s degree at Aurora University and her Master’s degree in counseling psychology from Lewis University in Romeoville. Ashley has over 10 years of experience with adults and adolescents, treating various mental health and substance abuse issues in a variety of settings.
Ashley is passionate about the collaborative care model. She believes it is important to have early intervention to minimize symptoms and have integrated care with providers to treat all aspects of health and improve quality of life.
MIKE SOUCIE, LCSW
 Mike is a Social Worker who serves as the Behavioral Care Coordinator at Gardner Healthcare Center and Channahon Healthcare Center.
Mike is a Social Worker who serves as the Behavioral Care Coordinator at Gardner Healthcare Center and Channahon Healthcare Center.
Mike earned his master’s degree from Southern Illinois University Edwardsville and his bachelor’s degree from the University of Iowa. Mike has 5 years of experience counseling adults and adolescents.
Mike maintains a passion for physical and mental wellness. He is a firm believer in the Collaborative Care Model as an innovative way to address mental and physical health symptoms in order to maximize patients’ quality of life.
REBECCA TELLEZ
 Rebecca Tellez is a mental health counselor who serves as the Pediatric Behavioral Care Coordinator under the Care Collaborative Model.
Rebecca Tellez is a mental health counselor who serves as the Pediatric Behavioral Care Coordinator under the Care Collaborative Model.
Rebecca has been employed by Morris Hospital since 2022 and serves as the first Pediatric Behavioral Care Coordinator to join the Care Collaborative Model. She has a master’s degree from Argosy University and bachelor’s degree from Loyola University.
Rebecca has 10+ years of experience with counseling and case management to a diverse group of patients across all demographics. Currently, she works with children and adolescents with a wide range of mental health concerns.
Rebecca believes greatly in the connection between mental and physical health, and finds this model of integrated care within pediatrics to be ideal for patients (and parents alike) to improve their overall health and well-being.
PSYCHIATRISTS
The Psychiatric Consultant is an expert consultant to the PCP and the Behavioral Care Coordinator. The team psychiatrist is available to advise your care team about diagnostic questions or treatment options, especially if you don’t improve with your initial treatment. The Behavioral Care Coordinator meets and consults regularly with the Psychiatric Consultant to talk about the progress of patients in the program and to think about treatment options.
THOMAS FREEMAN, M.D., CHILD & ADOLESCENT PSYCHIATRY
 Dr. Thomas Freeman is a board-certified Child and Adolescent Psychiatric physician with Morris Hospital and Healthcare Centers.
Dr. Thomas Freeman is a board-certified Child and Adolescent Psychiatric physician with Morris Hospital and Healthcare Centers.
Dr. Freeman serves as a psychiatric consultant to the behavioral care coordinators, primary care providers, and pediatricians for children and adolescents in the hospital’s Integrated Behavioral Health Program.
He completed his residency training at the University of Texas Medical School for General Psychiatry in 1989 and Washington University for Child and Adolescent Psychiatry in 2011. He received his Doctor of Medicine at the University of Texas Medical Branch in 1985.
He started his practice in general psychiatry and transitioned into child and adolescent psychiatry in 2011 after seeing a significant need in that population in underserved areas in rural Arkansas where he was practicing at the time.
NELLY NORRELL, MD, PSYCHIATRY
 Dr. Nelly Norrell is a board-certified psychiatric medicine physician with Morris Hospital & Healthcare Centers.
Dr. Nelly Norrell is a board-certified psychiatric medicine physician with Morris Hospital & Healthcare Centers.
Dr. Norrell serves as a psychiatric consultant to the behavioral care coordinators and primary care providers in the hospital’s Integrated Behavioral Health Program.
She completed her residency training at the University of Virginia, and previously received her Doctor of Medicine at the University of Arkansas for Medical Sciences in 2007. She specializes in geriatric psychiatry and completed her fellowship in 2021.
PATIENT RESOURCES
MEDICAL DIRECTOR OF INTEGRATED BEHAVIORAL HEALTH
Dr. Jennifer Thomas , MD, FASAM, is a board-certified physician in family medicine and addiction medicine and currently serves as Medical Director of Integrated Behavioral Health at Morris Hospital. She completed her medical degree at SIU School of Medicine in Springfield, IL in 2007, and completed her family medicine residency at Hinsdale Hospital outside Chicago in 2010.
, MD, FASAM, is a board-certified physician in family medicine and addiction medicine and currently serves as Medical Director of Integrated Behavioral Health at Morris Hospital. She completed her medical degree at SIU School of Medicine in Springfield, IL in 2007, and completed her family medicine residency at Hinsdale Hospital outside Chicago in 2010.
Dr. Thomas completed the University of California Irvine Train New Trainers Primary Care Psychiatry Fellowship in 2018. As a leader in developing partnerships between academic research settings and community-based providers, Dr. Thomas works closely with the University of Washington AIMS Center. Dr. Thomas serves as Project Lead for Morris Hospital’s partnership with the AIMS Center’s NIMH-sponsored research study CHAMP: Collaborating to Heal Addiction and Mental Health in Primary Care. As an advocate for increasing access to medication for Opioid Use Disorder, particularly in rural settings, Dr. Thomas was part of an inaugural cohort of 5 IL physicians in 2021 supported by ISAM to become board certified in addiction medicine through the ABPM Practice Pathway.
Dr. Thomas is currently accepting patients with primary care psychiatry and/or addiction concerns. She sees patients at the Braidwood Healthcare Center of Morris Hospital and the Gardner Healthcare Center of Morris Hospital.
PRIMARY CARE PSYCHIATRY FELLOWSHIP PROVIDERS
Morris Hospital and Healthcare Centers has embraced innovative solutions to help meet the behavioral health needs of our patients. Thanks to the generous support of the Morris Hospital Auxiliary and Foundation, Morris Hospital primary care providers received scholarship funding to participate in a primary care psychiatry fellowship. The University of California Irvine Train New Trainers Primary Care Psychiatry fellowship is a year-long clinical education program for primary care-oriented trainees and providers who wish to receive advanced training in primary care psychiatry.
The following five Morris Hospital providers have completed this Primary Care Psychiatry Fellowship training:
MEDICATION FOR OPIOID USE DISORDER
Medication for Opioid Use Disorder (MOUD) are evidence-based, FDA-approved medications that medical providers can prescribe to help treat Opioid Use Disorder (OUD). Many primary care providers now prescribe MOUD.
In order to improve access to MOUD care, Kathy Ulivi and Dr. Jennifer Thomas participated in the 2021 Carle Health OUD Treatment Fellowship ECHO® Program. Funded by the Illinois Substance Use Prevention and Recovery (SUPR) Agency, this training opportunity aims to increase access to medication for opioid use disorder in Illinois, with a special focus on primary care providers in communities with limited access to MOUD.
If you or someone you know would like more information on Medication for Opioid Use Disorder (MOUD) or other substance use disorder treatment options, please call 815-237-0413.
CHAMP STUDY
Morris Hospital & Healthcare Centers is participating in a three-year clinical trial funded by the National Institute of Mental Health to study the effectiveness of using integrated care – the combination of primary and mental health care in one setting – to treat opioid use disorder (OUD). Opioids include both prescription painkillers as well as certain street drugs, such as heroin. The University of Washington’s AIMS Center is facilitating the study called Collaborating to Heal Opioid Addiction and Mental Health in Primary Care (CHAMP) as part of a $19 million effort to study opioid addiction. Morris Hospital will provide four of the 24 primary care clinics that are partnering with the AIMS Center.
HELPFUL RESOURCES
- COLLABORATIVE CARE: http://aims.uw.edu/collaborative-care/
- CHAMP STUDY: https://champ.psychiatry.uw.edu/
